This is the case of a young 20 yo patient with PMH of asthma who presents from rehab with progressive low grade fevers, leukocytosis, and increasing transaminitis.
Back Story: The patient had a very recent 2 month hospital course preceding rehab for a bad case of status asthmaticus requiring mechanical ventilation with eventual trach and PEG. The patient also had enterococcus bacteremia with septic shock (from a presumed GI source), an ulcer/UGIB, CMV viremia, and elevated transaminitis to 200s (nl Alk phos, bili 6.0). An MRCP and liver biopsy was done which showed bl intrahepatic ductal dilation without fibrosis and a “beads on string” morphology. The patient left to rehab for severe deconditioning and then developed the above chief complaint with LFTs reaching the 900s with alk phos in the 2000s, TB 33 with direct in 20s!
On presentation, the patient had no symptoms of pruritis, acholic stools, abd pain, n/v, altered mental status but had stable loose stool from Tube feeds with exam significant only for being neon yellow and abd distention. Labs were significant for WBC 9.7, Hgb 7.9 bl, NAGMA, and LFTs as above with relatively normal albumin, INR liver function tests. The patient had a repeat MRCP which showed the same process and was ultimately diagnosed with ischemic cholangiopathy?!?! Although PSC is still on the ddx vs some other autoimmune process. Interesting Case!
Teaching Topics:
- Ischemic Cholangiopathy:
- Focal or extensive damage to the bile ducts via low blood flow, AKA ischemic cholangitis
- Blood supply from where? The peribiliary vascular plexus (PBP) from the hepatic artery.
- When does this happen? There appears to be a latency period after the initial insult but often diagnosed by abnormal labs are found – high Alk phos and GGT with progressive cholestasis – sound familiar?
- Later – itching, jaundice, hepatocellular failure…
- Where does this happen? classically affects the middle third of the CBD >>hepatic duct confluence with intraphepatic ducts being less common
- How does this happen? hepatic artery chemotherapy (floxuridine), advanced AIDs (CD4 <100), liver transplantation (biliary strictures & necrosis of bile ducts), hereditary hemorrhagic telangietasia, radiotherapy, polyarteriris nodosa, atherosclerosis, s/p cholecystectomy (2/2 strictures), sickle cell disease, SLE, APLAS and all the vasculitis or thrombotic diseases
- How do I treat this? Depends on the cause. If ischemic, Restore that blood flow! If this occurs after liver transplant, then up to 30% need re-transplantation! Patients can develop chronic biliary duct obstruction and need to be treated with ADEK vitamin supplementation, control pruritis ie with ursodiol and ppx abx to prevent infection
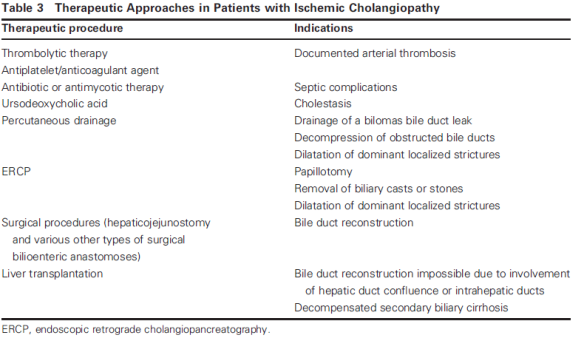
- Prognosis & Complications? If due to hepatic artery thrombosis – mortality is up to 50%. Causes of death include sepsis (tx with endoscopic intervention) , renal failure – [see GM MR on cholemic renal injury
- Focal or extensive damage to the bile ducts via low blood flow, AKA ischemic cholangitis