Tragic life update– I’m having laptop issues. Why can’t things just work when you want them to? You know you have a problem when switching on and off does not solve it.
Piece of advice for life– find a tech-savvy person who knows how to fix computers, hold on to them and keep them close.
Heart Block
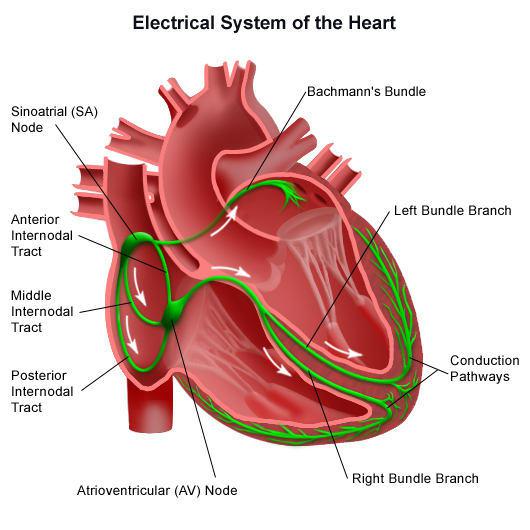 Definition: failure in normal conduction of electrical impulses from the atria to the ventricles due to blocks along the conduction system
Definition: failure in normal conduction of electrical impulses from the atria to the ventricles due to blocks along the conduction system
-Can be classified as:
1st degree AV block- the result of delayed atrioventricular conduction
2nd degree AV block– when some atrial impulses fail to reach the ventricles
-Wenckebach/ Mobitz type I block
-Mobitz type II block
3rd degree/ Complete AV block- all atrial activity fails to conduct to the ventricles
Aetiology/ risk factors:
–The common causes of heart block are coronary artery disease, cardiomyopathy, and, particularly in elderly people, fibrosis of the conducting tissue.
-Often a complication of a myocardial infarction
-Progression from 2nd degree AV block to complete heart block occurs more frequently following acute anterior MI and in Mobitz type II block.
Other causes:
-infection (e.g. rheumatic fever, infective endocarditis)
-drugs (e.g. digoxin, beta blockers, calcium channel blockers)
-metabolic (e.g. hyperkalaemia, cholestatic jaundice, hypothermia)
-infiltration of conduction system (e.g. sarcoidosis, cardiac neoplasms, amyloidosis)
-degeneration of conducting system.
Epidemiology: majority of the 250,000 pacemakers implanted annually are for heart block
Symptoms:
1st degree: asymptomatic
Wenckebach/ Mobitz type I block: usually asymptomatic
Mobitz type II and complete heart block: may cause Stokes-Adams attacks (syncope caused by ventricular asystole).
Classical description of a Stokes Adams attack is of collapse without warning associated with a loss of consciousness lasting seconds (~30). Individual is pale initially, pulseless but still breathing, and on recovery the patient becomes flushed. After about 15-20 seconds twitching may begin due to cerebral anoxia.
Other presentations include- dizziness, palpitations, chest pain and heart failure (dyspnoea, orthopnoea).
Signs: often normal. Examine for signs of the cause.
–Complete heart block: slow, large volume pulse; JVP may show large cannon a waves
–Mobitz type II and complete heart block: signs of reduced cardiac output e.g. hypotension, heart failure (bibasal crackles)
Investigations:
ECG (consider 24h ECG)–
1st degree AV block: Prolonged P-R interval (normal = 0.12-0.20s/ 3-5 small squares). No change in heart rate occurs.
2nd degree AV block
–Wenckebach/ Mobitz type I block: with each successive QRS, the P-R interval increases- until there is a non-conducted P wave (dropped QRS. The P-R interval then returns to normal and the cycle repeats itself.
–Mobitz type II block: P-R interval is constant. Ratio of AV conduction varies (2:1/3:1) but every few QRS complexes, there is a non-conducted P wave (dropped QRS). QRS complex is usually wide.
3rd degree/ Complete AV block: there is no relation between atrial and slower ventricular activity. There is complete dissociation between P waves and QRS complexes; they occur independently of one another.
Ventricular contractions are maintained by a spontaneous escape rhythm originating below the site of the block in the:
His bundle = narrow QRS complexes, 50-60 bpm, relatively reliable. Recent onset block due to transient causes e.g. ischaemia, and may respond to IV atropine without need for pacing.
Purkinje system = broad QRS complexes, slow (< 40bpm), unreliable, often associated with dizziness and blackouts (Stokes-Adams attacks)
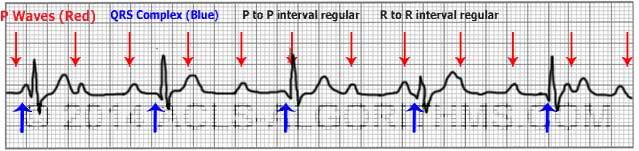
See how the P waves are regular and the QRS waves are regular, but there is no association between them i.e. there is no P wave before each QRS and a QRS after each P wave.
Look for other signs of cause e.g ischaemia
CXR- cardiomegaly, pulmonary oedema
Echo- wall motion abnormalities, aortic valve disease, vegetations.
Management:
-Stop beta blockers and calcium channel blockers (2nd, 3rd)
1st degree AV block– treatment unnecessary but observe closely as ~ 40% develop higher degrees of AV block.
2nd degree AV block
–Wenckebach/ Mobitz type I block = does not require permanent pacing unless poorly tolerated/ symptomatic, but needs to be monitored
–Mobitz type II block = should be paced, as carries high risk of developing sudden complete AV block
3rd degree/ Complete AV block = chronic complete heart block requires permanent pacing
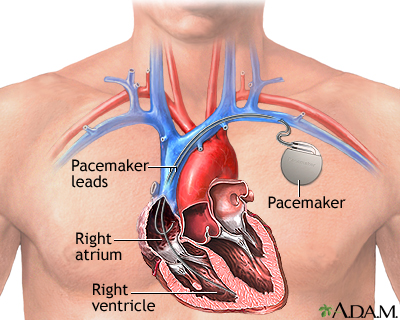
Permanent pacing:
Definition: pacemakers supply electrical initiation to myocardial contraction. The pacemaker lies subcutaneously where it may be programmed through the skin as necessary. Pacemakers usually last 5-10 years, but usually only the box needs replacing. Pacemakers can be single (atria or ventricles) or dual chamber.
ECG OF PACED RHYTHM -Pacing spikes occur before some of the P waves and the QRS complexes.
Indications:
-persistent AV block after anterior MI
-Mobitz type II AV block
-complete AV block (congenital, asymptomatic, Stokes-Adams attacks)
–symptomatic bradycardias e.g. sick sinus syndrome (sinus node dysfunction)
-heart failure (cardiac resynchronisation- symptomatic HF, LVEF < 35% = biventricular pacing +/- atrial lead +- combined with defibrillator)
-drug-resistant tachyarrhythmias
Complications:
-wound bleeding/ haematoma, wound infection
-dislodgement, malfunctioning
–pacemaker syndrome– in single chamber pacing, retrograde conduction to atria, which contract during ventricular systole so there is backflow in the pulmonary veins leading to decreased cardiac output, dyspnoea, palpitations, malaise and syncope.
–pacemaker tachycardia-in dual chamber pacing, a short circuit-loop goes between the electrodes causing an artificial WPW-like syndrome.
Acute blocks e.g. secondary to anterior MI can be considered for temporary (external pacing)
-After an acute anterior MI, prophylactic temporary cardiac pacing (external pacing) is required in Mobitz type I and Mobitz type II AV block and complete AV block. (IV atropine may be administered)
-However, it may in some cases be more efficient to arrange prompt, definitive pacing rather than temporary transvenous pacing.
-Post-MI, complete heart block usually resolves within a few days. Pacing may not be necessary after inferior MI if narrow QRS and reasonably stable with pulse > 40-50.
Complications:
–Stokes-Adams attacks
–Heart failure
-Asystole, cardiac arrest
Prognosis: Mobitz type II and complete heart block usually indicate serious underlying cardiac disease
References: Kumar and Clarke’s, Cheese & Onion, Rapid Medicine, GPNotebook
Advertisements Share this: