Topic: “The Opioid Epidemic”, QI perspective
Just a reminder, MEQAPI stands for Monitoring & Evaluation, Quality Assurance, and Process Improvement, and you can visit us at http://www.meqapi.org.
News articles sketch a chilling picture: Opioid-related death is quickly becoming the “modern plague” and surpassing cancer, heart disease, and motor vehicle accidents in those under 50 years. As a result, drug related deaths are now the number one cause of death in people under 50 in America.
We are expecting 59,000 deaths from opioid overdose this year, a 10% climb over 2016. Rural areas and low SES populations groups are the hardest hit, but the epidemic is spreading to all demographics. Opioid dependence is now seen as a leading risk factor in all surgeries (risk factor of 6%).
Physician’s Weekly have kindly shared the following pertinent articles (some with CME credits):
- #PWChat Recap: A Look at the U.S. Opioid Epidemic
- Video CME/CE: Pain Management & Opioids, With ZDoggMD t
- CME/CE: Guidance on Opioid Prescribing for Patients with Chronic Pain
- CME/CE: Initial Opioid Use & Long-Term Risks
- Filling Prescriptions After Opioid-Related Hospitalizations
- Reducing Opioid-Related Visits
- Surgery & Opioid Dependence Risk
- Opioid Treatment Programs & Older Adults
We will take a QI approach, and discuss the topic using each of the typical arms of the basic Quality Improvement Ishikawa diagram to guide and support discussion. An Ishikawa diagram will be provided ahead of time and during the chat.
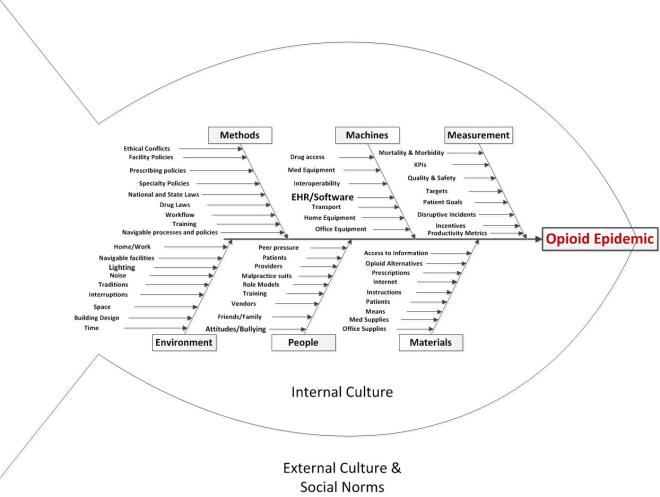
Participants will bring their own experiences, perspectives, and expectations to the discussion, but the topics might break down something along these lines:
-
- Methods
- Policies: office, organization, or national policies, including HIPAA, Physician assisted death policies, etc
- Workflow: how things are done including new patient onboarding, care provision, care coordination, ordering/prescribing, billing, patient transfer, etc.
- Workload: demands of the job, and whether they exceed the resources and ability to meet the demand.
- Human Resources Policies, and variation in expectations regarding women and men in the work setting and career progression
- Traditions and memes
- Incompatible drug and pain policies
- Ability to navigate drug laws, policies, and processes
- Machines (e.g. equipment, EHR)
- Medical or office equipment
- Home equipment specific to the patient condition
- Integration/interoperation with other office or medical systems, or user personal health records
- Drug access
- People
- Staffing: sufficient and qualified staff
- Training: base training, ongoing training, CME, and patient or carer training
- Attitudes: staff attitudes
- Fatigue and stress
- Values and traditions
- Friends and family
- Role Models
- Management styles
- Malpractice litigation
- Materials
- Patients: as the “raw material” of the medical process. Patients may come with a range of attitudes, health problems, life situations, and ability to comply with treatment that are challenging and stressful.
- Supplies: medical or office, or self-provided materials, uniforms, personal safety equipment.
- Data: ability to securely share with correct patient, specialist, lab, etc
- Internet sources
- Employment Handbook
- Discharge info packets
- Explanation of Benefits sheets
- Opioid alternatives
- Measurement
- Health outcomes, morbidity and mortality, birth defects
- KPIs: operational metrics required by practice, local government, state, federal
- Quality and safety metrics
- Targets: set by practice, insurer, etc. as well as patient goals
- Incentives and rewards
- Adverse Effects reporting
- Disruptive Incidents reporting
- Productivity metrics
- Patient goals
- Environment
- Noise: distracting noises, sound levels too high, etc. due to computer systems
- Space: Cramped, uncomfortable work space etc. Gender segregated space
- Time: Too little time per patient or order, too little time in a day, too many demands
- Location: things where they should be on the screen, click distance, and location of workstation relative to point of care and patient
- Control: the degree to which the individual can control their workload and how to accomplish it
- Fairness: the perception that the burdens and rewards, the effort and outcomes are spread amongst stakeholders in an equitable way
- Architecture: location of work areas, gathering places, shared areas
- Ability to navigate the healthcare facility
- Methods
Some of the authors of the works cited above may be responding to the following topics, and participants are invited to describe their experiences, and offer their insights and observations.
Topics
Background
MEQAPI focuses on healthcare improvement, and in the spirit of shameless borrowing (and efficiency), takes existing perspectives from the IHI, AHRQ, and others.
To quote the IHI on what the Triple Aim encompasses:
The IHI Triple Aim is a framework developed by the Institute for Healthcare Improvement that describes an approach to optimizing health system performance. It is IHI’s belief that new designs must be developed to simultaneously pursue three dimensions, which we call the “Triple Aim”:
- Improving the patient experience of care (including quality and satisfaction);
- Improving the health of populations; and
- Reducing the per capita cost of health care.
The six domains of care quality (STEEEP) mapped out by the Agency for Healthcare Research and Quality (AHRQ) are foundational to healthcare improvement. All care, and by inference quality measures, should be focused on being Safe, Timely, Effective, Efficient, Equitable, and Patient Centered. We add “Affordable” to this – STEEEPA
The MEQAPI tweetchat aims to give voice to a broad range of stakeholders in healthcare improvement, and it embraces everyone from administrators to zoologists, and includes physicians, nurses, researchers, bed czars, cleaners, and yes, patients and care-givers.
http://www.meqapi.org
Advertisements Share this: