This case is written by Dr. Rob Woods. He works in both the adult and pediatric emergency departments in Saskatoon and has been working in New Zealand for the past year. He is the founder and director of the FRCP EM residency program in Saskatchewan.
Why it MattersThis case requires learners to coordinate multiple components of care at once. A patient presenting with a STEMI requires urgent PCI, however they must also be stable enough to safely travel to the cardiac catheterization lab. This case emphasizes important adjuncts to STEMI management in an unstable patient, including:
- The utility of transcutaneous pacing and epinephrine infusion in the context of symptomatic bradycardia
- The importance of recognizing complete heart block as a complication of a STEMI
- The need for intubation in order to facilitate medication administration and safe transport in a PCI-requiring patient who presents with severe CHF or altered LOC
To be stated by the bedside nurse: “This 65-year-old woman came in with 1 hour of chest pressure and SOB. Her O2 sats were 84% on RA at triage, and they are now 90% with a non-rebreather mask. She’s also bradycardic at 30 and hypotensive at 77/40.”
Case SummaryA 65-year-old female is brought to the ED with chest tightness and SOB. On arrival, she will be found to have an inferior STEMI with resultant 3rd degree heart block and hypotension. The team will be expected to initiate vasopressor support and transcutaneous pacing. However, prior to doing so, the patient will develop a VT arrest requiring ACLS care. After ROSC, the team will need to initiate transcutaneous pacing and activate the cath lab for definitive management.
Download the case here: STEMI with Bradycardia ECG for the case found here: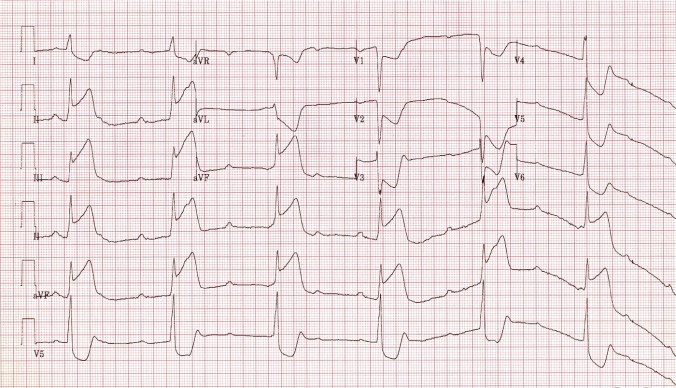
(ECG source: http://lifeinthefastlane.com/ecg-library/basics/inferior-stemi/)
CXR for the case found here:
(CXR source: https://www.med-ed.virginia.edu/courses/rad/cxr/pathology2Bchest.html)
Share this: