Lo and behold. Fogarty M, et al. Delayed Versus Early Umbilical Cord Clamping for Preterm Infants: A Systematic Review and Meta-Analysis. Am J Obstet Gynecol. 2017.
Some of the authors of the APTS trial have performed an updated systematic review, to put into context the results of their trial, which is exactly what should be done in such a circumstance. Their review includes the data from the trial I discussed in part 2, as they were available already (in the figure below they are listed as Duley 2016).
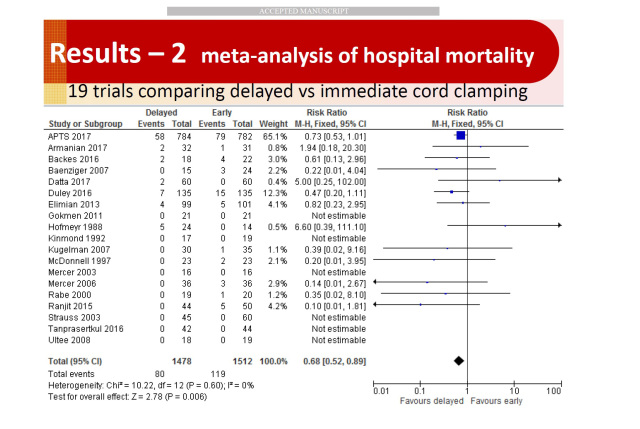
This review found 27 trials of delayed clamping that enrolled babies of less than 37 weeks gestation; most, as mentioned before, were tiny. When looking at the effects on mortality (for which there were 19 trials that reported the outcome) the results of the APTS trial were in fact not significant (at conventional levels of statistical significance) for death before discharge; which seems different to the published results, but the published results were for death before 36 weeks. As you can see from the figure below, death before discharge was 58 vs 79, rather than the 50 vs 70 for death before 36 weeks in the publication from the FPNEJM (the Formerly Prestigious New England Journal of Medicine); death before discharge had a relative risk of 0.73 95% CI 0.53 to 1.01.
There was little heterogeneity in the results, and, as you can see here, the mortality results depend largely on the latest 2 trials, which together contribute 77% of the weight for the meta-analysis.
 So where does this leave us? There is certainly no good evidence of a disadvantage of planning delayed clamping, compared to immediate clamping. Other outcomes: any IVH, severe IVH, PVL, a combination of serious persistent CNS abnormalities on ultrasound, late onset sepsis, NEC, RoP, were not different between early and late clamping. Hematocrit is increased by about 2.7%, and about 20% fewer babies receive a blood transfusion after delayed clamping. There are more babies with a hematocrit over 65% after delayed clamping, but no increase in partial exchange transfusions to treat them. Peak bilirubin levels are slightly higher after delayed clamping.
So where does this leave us? There is certainly no good evidence of a disadvantage of planning delayed clamping, compared to immediate clamping. Other outcomes: any IVH, severe IVH, PVL, a combination of serious persistent CNS abnormalities on ultrasound, late onset sepsis, NEC, RoP, were not different between early and late clamping. Hematocrit is increased by about 2.7%, and about 20% fewer babies receive a blood transfusion after delayed clamping. There are more babies with a hematocrit over 65% after delayed clamping, but no increase in partial exchange transfusions to treat them. Peak bilirubin levels are slightly higher after delayed clamping.
I remain a little sceptical about the advantages of delayed clamping beyond reducing transfusion requirements, the impact on mortality is basically from one trial (APTS) with an effect on mortality which might have been due to chance (p=0.07 from the Yates corrected chi-square), with a contribution from the Duley trial, with an individual p value of 0.12. I am should also sceptical about the relevance to my practice of a study such as Ranjit 2015, who only enrolled infants between 30 and 36+6/7 gestation who did not need resuscitation, but had a 10% mortality in the early clamping group.
For relatively uncommon events we often have to rely on systematic review to be confident about the impact of an intervention, but meta-analysis of multiple very small trials is known to be problematic, and often inflates the apparent impact of an intervention. I think though it is unlikely we will have more large trials of planned delayed clamping in the very preterm compared to early clamping. I did a quick search of clinicaltrials.gov and couldn’t find such a trial, there are, in contrast, trials comparing cord milking to delayed clamping.
Reassuring is the subgroup analysis of babies of less than 28 weeks gestation, which also showed a decrease in mortality (RR=0.7, 95% CI 0.51, 0.95), but that includes only 996 babies from 3 trials, (871 of whom were from APTS).
Why might delayed clamping reduce mortality without reducing individually any of the primary causes of mortality? It is possible that an improved perinatal adaptation could lead to more stable babies in the first hours of life that decreases a whole spectrum of later causes of death, but it is hard to understand why deaths from late onset sepsis would be reduced, for example.
In my opinion, if we take into account all the limitations in these data I am not absolutely convinced that delayed clamping leads to decreased mortality, but I think that, on balance, it probably does.
My take home message is that planned delayed cord clamping should now be the standard for the preterm infant. The benefits on reduction of transfusion without any harm detected for the baby or the mother, and a probable reduction in mortality, are important, and there is no signal for an adverse impact.
What next? The Duley trial was, of course, quite different to APTS, examining resuscitation with an intact placental circulation. The extra organization and equipment required for this approach should be justified, I believe, by a trial comparing A. planned delayed clamping at 1 minute but with clamping as soon as the baby is thought to need active resuscitation to B. planned delayed clamping at 2 minutes (or more) with active intervention as soon as thought necessary, the cord only being clamped early if there are technical obstacles.
I don’t think you should, ethically, randomize preterm babies to planned immediate clamping. The alternative would be to only randomize infants who were thought to need immediate intervention, and to compare immediate clamping to resuscitation with an intact cord, but that I think would be technically more difficult to do, and would probably require a waiver of consent.
Share this:





